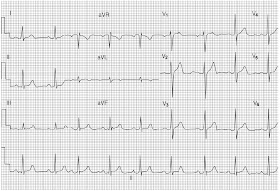
• Normal ECG recording consists of P wave (atrial beat), followed by QRS, ST and T wave (ventricular beat).
• Capital letter P, Q, R, S, T—indicates large wave (> 5 mm).
• Small letter p, q, r, s, t—indicates small wave (< 5 mm).
TYPES OF WAVES IN ECG
• P — Deflection produced by atrial depolarization.
• QRS — Deflection produced by ventricular depolarization.
• Q (q) — First negative deflection produced by ventricular depolarization. It precedes R wave.
• R(r) — First positive deflection produced by ventricular depolarization.
• S(s) — Negative deflection after R wave produced by ventricular depolarization.
• T — Indicates ventricular repolarization.
OTHER WAVES
• J — At the beginning of ST segment.
• U — Not always seen. When present, it follows T wave, preceding the next P wave. It indicates repolarization of interventricular septum or slow repolarization of the ventricles.
INTERVALS IN ECG
• PR interval — Distance between the beginning of P to beginning of QRS (Q), ideally called PQ interval.
• PP interval — Distance between two successive P waves. In sinus rhythm, P-P interval is regular.
• RR interval — Distance between two successive R waves. In sinus rhythm, R-R interval is regular.
• QT interval — Distance interval between the beginning of Q wave and the end of T wave.
SEGMENT IN ECG
ST—Distance from the end of QRS complex to the beginning of T wave. It indicates the beginning of ventricular repolarization. Normally, it is in isoelectric line, but may vary from – 0.5 to + 2 mm in chest leads.
It is important here to note that:
• Ventricles contain majority of the heart muscles (left ventricle contains more than the right). So, QRS is larger than P wave.
• Atrial repolarization is small and is buried in QRS. So, it is not seen in ECG (No wave is seen due to atrial repolarization in ECG).
P WAVE
Characters of Normal P Wave
• P wave results from spread of electrical activity through the atria.
• Width or duration (in time, horizontally) - 0.10 sec (2.5 small sq.).
• Height - 2.5 mm (2.5 small sq.). (Height × Duration = 2.5 × 2.5 small squares).
• P wave is better seen in LII, as atrial depolarization is towards LII (also seen in V1), because the impulse spread from right to left atrium.
• P wave is upright in all leads, mainly LI, LII and aVF (except aVR). (P is inverted in aVR and occasionally in aVL).
• P wave in V1 may be biphasic (equal upward and downward deflection), notched and wide. (Activation of right atrium produces positive component and activation of left atrium produces negative component).
• Normal P is rounded, neither peaked nor notched.
Abnormalities of P Wave
P wave may be:
• Absent.
• Tall or small.
• Wide, notched, biphasic.
• Inverted.
• Variable and multiple.
Causes of absent P wave
• Atrial fibrillation (P is absent or replaced by fibrillary f wave).
• Atrial flutter (P is replaced by flutter wave, which shows saw-tooth appearance).
• SA block or sinus arrest.
• Nodal rhythm (usually abnormal, small P wave).
• Ventricular ectopic and ventricular tachycardia.
• Supraventricular tachycardia (P is hidden within QRS, due to tachycardia).
• Hyperkalemia.
• Idioventricular rhythm.
Causes of tall P wave
• Tall P is called P pulmonale (height > 2.5 mm, i.e. > 2.5 small squares).
• It is due to right atrial hypertrophy or enlargement.
Causes of small P wave
• Atrial tachycardia.
• Atrial ectopic.
• Nodal rhythm (high nodal).
• Nodal ectopic (high nodal).
Causes of wide P wave
• Broad and notched P is called P mitrale (duration > 0.11 sec, or > 2.5 small squares).
• It is due to left atrial hypertrophy or enlargement.
• In V1, P wave may be biphasic with a small positive wave preceding a deep and broad negative wave (indicates left atrial enlargement or hypertrophy).
Causes of inverted P wave (negative in LI, LII and aVF)
• Incorrectly placed leads (reversed arm electrodes).
• Dextrocardia.
• Nodal rhythm with retrograde conduction.
• Low atrial and high nodal ectopic beats.
Causes of variable P waves
Presence of variable P waves indicates wandering pacemaker.
Causes of multiple P waves (consecutive 2 or more)
• A-V block (either partial or complete heart block).
• SVT with AV block.
P-R INTERVAL
Characters of Normal P-R Interval
• It is the distance between the onset of P wave to the beginning of Q wave (if Q wave is absent, then measure up to the onset of R wave).
• It is the time required for the impulse to travel from SA node to the ventricular muscle. (The impulse is transmitted to ventricle via AV node).
• P-R interval varies with age and heart rate. (P-R interval is short, if the heart rate is increased and long, if heart rate is decreased).
• Normal PR interval—0.12 to 0.20 sec (maximum 5 small squares).
— In children, upper limit is 0.16 sec.
— In adolescent, upper limit is 0.18 sec.
— In adult, upper limit is 0.22 sec.
• P-R is short, if it is < 0.10 sec and long, if it is > 0.22 sec.
Abnormalities of P-R Interval
PR interval may be:
• Prolonged.
• Short.
• Variable.
Prolonged P-R interval (> 0.2 second): It is due to first degree heart block. Causes are:
• Ischemic heart disease (occasionally, inferior MI).
• Acute rheumatic carditis.
• Myocarditis (due to any cause).
• Atrial dilatation or hypertrophy.
• Hypokalemia.
• Drugs—digitalis toxicity, quinidine, occasionally β-blocker, calcium channel blocker (verapamil).
Short P-R interval (< 0.12 second): Causes are:
• Wolff-Parkinson-White (WPW) syndrome. In this case, there is delta wave.
• Lown-Ganong-Levine (LGL) syndrome. In this case, there is no delta wave.
• Nodal rhythm.
• Nodal ectopic (high nodal).
• Occasionally, if dissociated beat is present and also in infant, steroid therapy.
Variable P-R interval: Causes are:
• Wenckebach’s phenomenon (Mobitz type I): There is progressive lengthening of P-R interval followed by a drop beat.
• Partial heart block (Mobitz type II): PR interval is fixed and normal, but sometimes P is not followed by QRS.
• 2 :1 AV block: Alternate P wave is not followed by QRS.
• Complete AV block: No relation between P and QRS.
• Wandering pacemaker: Variable configuration of P.
Q WAVE
Characters of Normal Q Wave
• Q wave is usually absent in most of the leads. However, small q wave may be present in I, II, aVL, V5 and V6. This is due to septal depolarization.
• Small q may be present in LIII (which disappears with inspiration).
• Depth—< 2 mm (2 small squares).
• Width—1 small square.
• It is 25% or less in amplitude of the following R wave in the same lead.
Characters of Pathological Q Wave
• Deep > 2 mm (2 small squares).
• Wide > 0.04 sec or more (> 1 mm or 1 small square).
• Should be present in more than one lead.
• Associated with loss of height of R wave.
• Q wave should be > 25% of the following R wave of the same lead.
Causes of Pathological Q Wave
• Myocardial infarction (commonest cause).
• Ventricular hypertrophy (left or right).
• Cardiomyopathy.
• LBBB.
• Emphysema (due to axis change or cardiac rotation).
• Q only in LIII is associated with pulmonary embolism (SI, QIII and TIII pattern).
Remember the following points:
• Q wave in V1, V2 and V3 may be seen in LVH and may be mistaken as old myocardial infarction.
• Abnormal Q wave in LIII may be found in pulmonary embolism.
• Abnormal Q wave in LIII and aVF may be found in WPW syndrome (confuses with old inferior myocardial infarction).
R WAVE
Characters of Normal R Wave
• It is the first positive (upward) deflection, due to ventricular depolarization.
• Duration < 0.01 sec.
• R wave usually small (< 1 mm) in V1 and V2. It increases progressively in height in V3 to V6 (tall in V5 and V6), i.e. R is small in V1 and V2, tall in V5 and V6.
Normal Height of R Wave
• aVL < 13 mm.
• aVF < 20 mm.
• V5 and V6 < 25 mm.
(If R wave is > 25 mm, it is always pathological).
Abnormalities of R Wave
R wave may be:
• Tall.
• Small.
• Poor progression.
Causes of tall R wave
1. Left ventricular hypertrophy (in V5 or V6 > 25 mm, aVL >13 mm, aVF > 20 mm).
2. In V1, tall R may be due to:
• Normal variant.
• Right ventricular hypertrophy (RVH).
• True posterior myocardial infarction.
• WPW syndrome (type A).
• Right bundle branch block.
• Dextrocardia.
Causes of small R wave: Looks like low voltage tracing.
• Incorrect ECG calibration (standardization).
• Obesity.
• Emphysema.
• Pericardial effusion.
• Hypothyroidism.
• Hypothermia.
R wave progression: The height of R wave gradually increases from V1 to V6. This phenomenon is called R wave progression.
Poor progression of R wave: Normally, amplitude of R wave is tall in V5 and V6. In poor R wave progression, amplitude of R wave is progressively reduced in V5 and V6.
Causes are:
• Anterior or anteroseptal myocardial infarction.
• Left bundle branch block.
• Left ventricular hypertrophy (though R is tall in most cases).
• Dextrocardia.
• Cardiomyopathy.
• COPD.
• Left sided pneumothorax.
• Left sided pleural effusion (massive).
• Marked clockwise rotation.
• Chest electrodes placed incorrectly.
• Deformity of the chest wall.
• Normal variation.
S WAVE
Characters of Normal S Wave
• It is the negative deflection after R wave (1/3rd of R wave).
• Normally, deep in V1 and V2 as impulse is going to the muscles of left ventricle then to the right ventricle.
• Progressively diminished from V1 to V6 (small S wave may be present in V5 and V6).
• In V3, R and S waves are almost equal (corresponds with interventricular septum).
QRS COMPLEX
Characters of Normal QRS Complex
• QRS complex represents depolarization of ventricular muscles.
• Depolarization of left ventricle contributes to main QRS (as the left ventricle has 2 to 3 times mass of right ventricle).
• QRS is predominantly positive in leads that look at the heart from left side—L1, aVL, V5 and V6.
• It is negative in leads that look at the heart from the right side—aVR, V1 and V2.
• In V1, S is greater than R.
• In V5 and V6, R is tall.
• QRS appears biphasic (part above and part below the base line) in V3 and V4.
• Normal duration of QRS is 0.08 to 0.11 second (< 3 small squares) and height < 25 mm.
Various Forms and Components of QRS Complex
• Q wave: Initial downward deflection.
• R wave: Initial upward deflection.
• S wave: Downward deflection after R wave.
• rS complex: Small initial r wave, followed by large S wave.
• RS complex: A complex with R and S wave of equal amplitude.
• Rs complex: A large R wave followed by a small s wave.
• qRS complex: Small initial downward deflection, followed by a tall R which is followed by a large S.
• Qr complex: Large Q, followed by a small r.
• QS complex: Complex with complete negative deflection (no separate Q and S).
• rSr complex: Small r, then deep S, followed by small r.
• RSR complex: Tall R, then deep S, followed by tall R.
• RR complex: When deflection is completely positive and notched (M pattern).
Abnormalities of QRS Complex
QRS may be:
• High voltage.
• Low voltage.
• Wide.
• Change in shape.
• Variable.
Causes of high voltage QRS
• Incorrect calibration.
• Thin chest wall.
• Ventricular hypertrophy (right or left or both).
• WPW syndrome.
• True posterior myocardial infarction (in V1 and V2).
Causes of low voltage QRS (< 5 mm in LI, LII, LIII and < 10 mm in chest leads)
• Incorrect calibration.
• Thick chest wall or obesity.
• Hypothyroidism.
• Pericardial effusion.
• Emphysema.
• Chronic constrictive pericarditis.
• Hypothermia.
Causes of wide QRS (> 0.12 second, 3 small squares)
• Bundle branch block (LBBB or RBBB).
• Ventricular ectopics.
• Ventricular tachycardia.
• Idioventricular rhythm.
• Ventricular hypertrophy.
• Hyperkalemia.
• WPW syndrome.
• Pacemaker (looks like LBBB with spike).
• Drugs (quinidine, procainamide, phenothiazine, tricyclic antidepressants).
Causes of changes in shape of QRS
• Right or left bundle branch block (slurred or M pattern).
• Ventricular tachycardia.
• Ventricular fibrillation.
• Hyperkalemia.
• WPW syndrome.
Causes of variable QRS
• Multifocal ventricular ectopics.
• Torsades de pointes.
• Ventricular fibrillation.
ST SEGMENT
Characters of Normal ST Segment
• Measured from the end of S to the beginning of T wave. It represents beginning of ventricular repolarization.
• Normally, it is in isoelectric line (lies at same level of ECG baseline).
• ST elevation is normal up to 1 mm in limb leads and 2 mm in chest leads (mainly V1 to V3).
• In Negroes, ST elevation of 4 mm may be normal, which disappears on exercise.
• Normally, ST segment may be depressed, < 1mm.
Abnormalities of ST Segment
ST segment may be:
• Elevated.
• Depressed.
Causes of ST elevation (> 2 mm)
• Recent myocardial infarction (ST elevation with convexity upward).
• Acute pericarditis (ST elevation with concavity upward, chair shaped or saddle shaped).
• Prinzmetal’s angina (ST elevation with tall T).
• Ventricular aneurysm (persistent ST elevation).
• Early repolarization (high take off).
• Normal variant in Africans and Asians.
• May be in hyperkalemia.
Causes of ST depression (below the isoelectric line)
• Acute myocardial ischemia (horizontal or down slope ST depression with sharp angle ST-T junction).
• Ventricular hypertrophy with strain (ST depression with convexity upward and asymmetric T inversion).
• Digoxin toxicity (sagging of ST depression—like thumb impression, also called reverse tick).
• Acute true posterior myocardial infarction (in V1 and V2), associated with dominant R and tall upright T wave.
Early repolarization (high take-off)
• It is a benign, normal finding in young healthy person, more in black males.
• It is seen in chest leads, commonly V4 to V6 (rarely, in other chest lead).
• ST elevation is usually associated with J point elevation.
• It is not associated with inversion of T wave or abnormal Q wave.
Remember the following points:
• Early repolarization syndrome confuses with acute myocardial infarction and acute pericarditis.
• To differentiate from these, detail history, serial ECG tracing (that shows no change) and comparison with old ECG are helpful.
T WAVE
Characters of Normal T Wave
• It indicates ventricular repolarization.
• Follows S wave and ST segment.
• Upright in all leads, except aVR.
• Usually, more than 2 mm in height.
• May be normally inverted in V1 and V2.
• Normally, not more than 5 mm in standard leads and 10 mm in chest leads.
• Minimum 1/4th of R wave of the same lead.
• Tip of T is smooth (rounded).
Abnormalities of T Wave
T wave may be:
• Inverted.
• Tall peaked, tented.
Causes of T inversion
• Myocardial ischemia and infarction.
• Subendocardial myocardial infarction (non-Q wave myocardial infarction).
• Ventricular ectopics.
• Ventricular hypertrophy with strain.
• Acute pericarditis.
• Cardiomyopathy.
• Myxoedema.
• Bundle branch block.
• Drugs (digitalis, emetine, phenothiazine).
• Physiological (smoking, anxiety, anorexia, exercise, after meal or glucose).
Causes of tall peaked T wave
• Hyperkalemia (tall, tented or peaked).
• Hyperacute myocardial infarction (tall T wave).
• Acute true posterior myocardial infarction (tall T in V1 to V2).
• May be normal in some Africans and Asians.
Causes of small T wave
• Hypokalemia.
• Hypothyroidism.
• Pericardial effusion.
U WAVE
Characters of Normal U Wave
• It follows T wave.
• It may be present in normal ECG. It is smaller and in the same direction of the preceding T wave.
• It represents slow repolarization of interventricular septum (Purkinje fibers, but actual genesis of U wave is still controversial).
• It is better seen in chest leads (V2 to V4).
• Normal amplitude is 1 mm (2 mm in athlete).
Abnormalities of U Wave
U wave may be:
• Inverted.
• Prominent.
Causes of inverted U wave
• Ischemic heart disease.
• Left ventricular hypertrophy with strain (hypertensive heart disease).
Causes of prominent U wave
• May be normally present (usually small).
• Hypokalemia (commonest).
• Bradycardia.
• Ventricular hypertrophy.
• Hyperthyroidism.
• Hypercalcemia.
• Drugs (phenothiazine, quinidine, digitalis).
Significance of large U wave: The patient is prone to develop torsades de pointes tachycardia.
QT INTERVAL
Characters of Normal QT Interval
• It is the distance from the beginning of Q wave (or R wave, if there is no Q wave) to the end of T wave. It represents the total time required for both depolarization and repolarization of the ventricles.
• Normal QT interval is 0.35 to 0.43 seconds.
• Its duration varies with heart rate, becoming shorter as the heart rate increases and longer as the heart rate decreases.
In general, QT interval at heart rate between 60 to 90/minute does not exceed in duration half the preceding RR interval.
• It is better seen in aVL (because there is no U wave).
• Corrected formula for real QT is:
QTc = QT/RR(underroot)
Abnormalities of QT Interval
QT interval may be:
• Short.
• Long.
Causes of short QT interval
• Digoxin effect.
• Hypercalcemia.
• Hyperthermia.
• Tachycardia
Causes of long QT interval
• Hypocalcemia.
• Bradycardia.
• Acute myocarditis.
• Acute myocardial infarction.
• Hypothermia.
• Drug (quinidine, procainamide, flecainide, amiodarone, tricyclic antidepressant, disopyramide, pentamidine).
• Cerebral injury (head injury, intracerebral hemorrhage).
• Hypertrophic cardiomyopathy.
• During sleep.
• Hereditary syndrome:
(a) Jervell-Lange Nielsen syndrome (congenital deafness, syncope and sudden death).
(b) Romano-Ward syndrome (same as above except deafness).
RHYTHM OF HEART
To see the rhythm—see the successive RR interval.
• If the RR interval is equal, it is called regular rhythm.
• If the RR interval is irregular, then it is called irregular rhythm.
Causes of Irregular Rhythm
1. Physiological: Sinus arrhythmia.
2. Pathological:
• Atrial fibrillation.
• Atrial flutter.
• Ectopic beat.
• SA block or sinus arrest.
• Atrial tachycardia with block.
• Second degree heart block.
• Ventricular fibrillation.
CHARACTERS OF SINUS RHYTHM
Sinus rhythm shows the following 5 characters:
- • P wave is of sinus origin (means characters of normal P wave).
- • P waves and QRS complexes are regular (that means P-P and R-R interval should be constant and identical).
- • Constant P wave configuration in a given lead.
- • P-R interval and QRS interval should be within normal limit.
- • Rate should be between 60 to 100 beats/min (atrial and ventricular rates are identical).





I started on COPD Herbal treatment from Ultimate Health Home, the treatment worked incredibly for my lungs condition. I used the herbal treatment for almost 4 months, it reversed my COPD. My severe shortness of breath, dry cough, chest tightness gradually disappeared. Reach Ultimate Health Home via their website at www.ultimatelifeclinic.com I can breath much better and It feels comfortable!
ReplyDelete